September 12, 2025
Frequently asked questions: Marburg virus disease
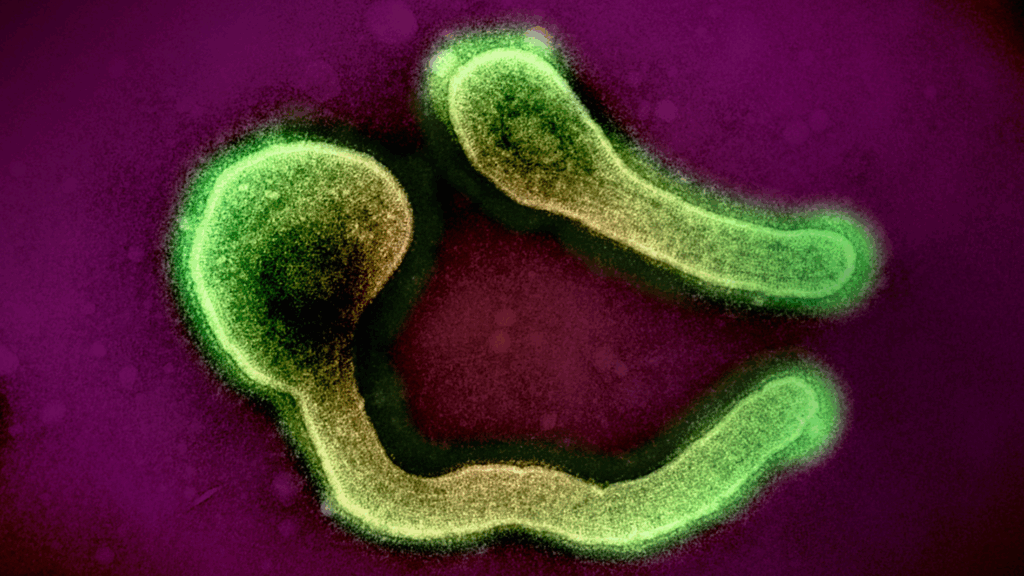
Learn more about Marburg virus, a filovirus that causes a severe hemorrhagic illness in humans.
Exactly what is Marburg virus (MARV)? At least 19 outbreaks of Marburg virus disease (MVD) have been reported since 1967, when two simultaneous outbreaks occurred in Germany and Serbia associated with imported African green monkeys from Uganda. Since then, MARV has continued to cause sporadic but deadly outbreaks across sub-Saharan Africa, including travel-related cases in the U.S. and Europe. Due to its high case fatality rate (CFR) and high potential to cause a public health emergency of international concern, MARV is a priority pathogen for which IAVI and our partners are developing a vaccine candidate as part of our emerging infectious disease (EID) vaccine program. Read more about our MARV vaccine development program.
Frequently asked questions
The pathogen MARV (viral species Orthomarburgvirus marburgense) causes MVD – a severe, often fatal, viral hemorrhagic fever – in humans and non-human primates. While disease is rare, many outbreaks have been recorded since it was identified in 1967 (the majority occurring in sub-Saharan Africa). With a CFR that ranges from 24% to 88% in past outbreaks, MVD is included in the World Health Organization (WHO) Pathogen Prioritization framework as a priority pathogen for which a vaccine is urgently needed.
MARV is often associated with Ebola virus (EBOV) as both are filoviruses in the same family and cause outbreaks with high CFRs. Although caused by two distinct viruses, MVD and Ebola virus disease (EVD) present clinically similar symptoms. It can be difficult to distinguish between MVD, EVD, and other similar infectious diseases – resulting in delayed diagnosis, reporting, and treatment.
MARV is zoonotic and presumed to be carried by Egyptian fruit bats. The virus is typically transmitted to humans when they come into contact with colonies of infected fruit bats in a mine or cave. This process is known as “zoonotic spillover.” Once introduced to a human population, the virus can then be transmitted from person to person via direct contact with a symptomatic MVD patient or their infectious bodily fluids. Infection from touching the bodies of the recently deceased is also possible. People are considered infectious for as long as the virus is found in their blood.
Once a person is infected with MARV, the incubation time before symptoms appear is two to 21 days. Early symptoms begin with a fever, malaise, headache, and other body aches. Symptoms then become increasingly severe and can include nausea, vomiting, and a rash. In later stages of the disease, patients may experience hemorrhaging (bleeding) from multiple sites, shock, and organ failure. Infected pregnant women may also experience miscarriage or stillbirth.
MVD may present similarly to other infectious diseases, so early detection is crucial. Infection must be confirmed using a laboratory blood test.
MVD can become fatal abruptly as death occurs most often between 8 and 9 days after symptom onset. For survivors, recovery can take months, and the virus can remain in their bodies for several weeks.
According to the WHO, 19 total outbreaks of MVD have been confirmed since 1967. In September 2024, Rwanda became the fifth new country in three years to experience its first outbreak.
People who work in mines or visit caves in areas where the virus is enzootic are at risk of initial exposure from Egyptian fruit bat colonies. Health workers, close contacts, family members, and people who are involved in burial ceremonies are at heightened risk after initial zoonotic transmission. People who have recently traveled to an area with an active outbreak may also have an elevated risk of infection. Pregnant women may also face an increased risk of severe disease compared with the general population.
No licensed vaccines or therapeutics are available for MVD. Treatment is limited to supportive care such as replacing blood components, balancing fluids and electrolytes, maintaining oxygen status and blood pressure, and organ support as needed. Currently, candidate monoclonal antibodies (mAbs) and antivirals are in development to improve MVD treatment options.
Several MARV vaccine candidates are in development, including IAVI and our partners’ recombinant vesicular stomatitis virus (rVSV) vector-based candidate. In 2024, this vaccine candidate was prioritized for review by a WHO Technical Advisory Group in response to a new MVD outbreak in Rwanda.
You can read more about IAVI’s MARV vaccine development efforts and our promising preclinical data here.
In the absence of a vaccine, MVD poses a serious public health risk. A combination of community engagement and outbreak control are priorities for the WHO and national health officials. Community engagement involves messaging that raises awareness of the risk factors associated with MVD, including bat-to-human transmission resulting from exposure in caves or mines and transmission within the community. It is essential to ensure that communities are well-informed about the nature of this disease and key outbreak containment measures: safe burial practices, good hygiene, and identification of close contacts. If an outbreak does occur, the WHO emphasizes case management, surveillance and contact tracing, good laboratory practices, infection prevention in health facilities, and social mobilization. However, more coordinated action and investment are needed to develop effective medical countermeasures that can either prevent an outbreak altogether or stop an active outbreak in its tracks.
https://www.who.int/health-topics/marburg-virus-disease#tab=tab_1
https://www.who.int/news-room/fact-sheets/detail/marburg-virus-disease
https://www.who.int/news-room/questions-and-answers/item/marburg-virus-disease
https://www.who.int/emergencies/disease-outbreak-news/item/2024-DON548
https://www.cdc.gov/marburg/about/index.html
https://www.cdc.gov/ebola/about/index.html
https://www.who.int/en/news-room/fact-sheets/detail/ebola-virus-disease
https://www.gov.uk/guidance/marburg-virus-disease-origins-reservoirs-transmission-and-guidelines